'Smart' Wound Dressing Delivers Meds, Monitors Temperature, Lights Up
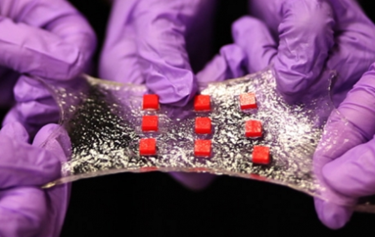
MIT Scientists have introduced a hydrogel-based bandage embedded with electronics and drug-delivering reservoirs for a wound-care solution that can monitor vitals (such as temperature), release drugs if needed, and light up if the medication is running low. The researchers say the stretchable material is more compatible with the body’s structure than traditional dressings, and it may be useful for applications both inside and outside the body.
Recent advances in biomedical hydrogels have increased their popularity among engineers looking to develop next-generation medical devices, such as contact lenses, drug delivery devices, and tissue engineering scaffolds. The softness, flexibility, and porosity of hydrogel’s structure is similar to organic tissue, making hydrogels uniquely biocompatible.
“Electronics are usually dry and hard, but the human body is soft and wet. These two systems have drastically different properties,” said Xuanhe Zhao, senior researcher and MIT associate professor of mechanical engineering, to MIT News. “If you want to put electronics in close contact with the human body for applications such as health care monitoring and drug delivery, it is highly desirable to make the electronic devices soft and stretchable to fit the environment of the human body.”
According to Zhao, the team faced two main challenges when developing its hydrogel: mechanical strength and ability to cling to porous surfaces. In order to ensure these characteristics, the team developed a hydrogel capable of dissipating the energy required to stretch it and chemically anchored to form covalent bonds with various surfaces.
When the team introduced its robust hydrogel last month, graduate student Hyunwoo Yuk told MIT News, “Basically, it’s tough, bonding water.”
For the next step in its research, the team incorporated the hydrogel with compatible electrical systems. In a study published in Advanced Materials, the researchers demonstrated different applications for a novel wound dressing that could track the temperature of the wound and release drugs from reservoirs that diffused through the hydrogel over an extended period of time. Embedded LED lights were programmed to light up when the reservoirs emptied.
Though the study proposed a wound-care application, Zhao speculated that the technology could also be applied to implanted glucose monitors and neural probes, somewhere down the road. Ordinary implants — said Zhao — run the risk of immune response or detaching internally, which can cause serious complications.
“With collaborators, we are proposing to use robust hydrogel as an ideal material for neural devices, because the hydrogel can be designed to possess similar mechanical and physiological properties as the brain,” said Zhao.
Bandages everywhere are due for an upgrade, and Digital Trends reported that several international research teams were looking for new ways to incorporate smart electronics into wound dressings. A German team is working on a bandage that changes colors in response to pH levels in the skin, and a team from UC Berkeley is developing a skin sensor that can detect a bedsore before it begins to form.
In a YouTube video, UC Berkeley engineer Michel Maharbiz explained that miniaturized technology and better understanding of human response will lead to a “more intelligent” bandage. “You can imagine a future—which is very close—where the bandage that you put on or the dressing that a surgeon uses will be able to report a lot of interesting information about the progress of that wound.”
