New "Muscle-On-A-Chip" Could Enable Patient-Specific Asthma Treatments
By Chuck Seegert, Ph.D.
Current methods of testing asthma drugs are often poor predictors of how they will perform in humans. To provide a tool for testing these drugs, Harvard researchers have developed a bench top test that uses human cells and may be more accurate than current methods.
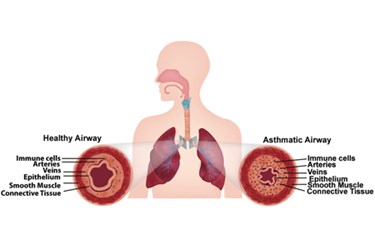
In the United States alone, many millions of people suffer from asthma, a chronic respiratory disease. Despite this large number, the medicines used to treat it are somewhat antiquated and have been around for some time. The disease affects patients differently and is somewhat patient-specific, which makes it difficult to find drugs for larger populations. Traditionally, animal models have been used to test potential treatments, but results from these models are somewhat tenuous. Generally, there is little certainty that they will translate into successful human treatments.
Finding a human relevant model that could help with this challenge was the goal of a Harvard engineering team. To do this, the team developed the “human airway muscle-on-a-chip” technology, according to a recent press release. The chip uses human smooth muscle cells to accurately replicate contraction in the human airway.
"Every year asthma costs many tens of billions of dollars, significant productivity due to lost work and school days, and even lives," said senior author Kevin Kit Parker, Ph.D., a core faculty member at Harvard's Wyss Institute for Biologically Inspired Engineering and Tarr Family Professor of Bioengineering and Applied Physics at the Harvard School of Engineering and Applied Sciences (SEAS), in the press release. "We were thrilled with how well the chip recapitulated the functioning of the human airway."
The “muscle-on-a-chip” device is made of a thin elastomeric layer, which gains its functionality through human smooth muscle cells that are cultured on it, according to a recent study published by the team in the Royal Society of Chemistry journal Lab On A Chip. When exposed to interleukin-13, the smooth muscle cells contract, curling the elastomeric layer — a contraction that replicates what has been seen in asthmatic bronchoconstriction. When exposed later to drugs called β-agonists, which are used to treat asthma, the cells were shown to relax — a behavior that closely mimics what is seen in the clinic.

Because the cells are cultured, they can be studied for protein expression, structural changes, and even functional changes. This advance may allow medicines to be developed for many patients who currently don’t respond to treatment.
"Asthma is one of the top reasons for trips to the emergency room — particularly for children, and a large segment of the asthmatic population doesn't respond to currently available treatments," said Wyss Institute founding director Don Ingber, M.D., Ph.D., in the press release "The airway muscle-on-a-chip provides an important and exciting new tool for discovering new therapeutic agents."
Developing in vitro tests that mimic certain physiologic settings is a practice that is accelerating in today’s research environment to increase accuracy and reduce costs. Very recently, in an article published on Med Device Online, a tumor-on-a-chip model was discussed that is used for testing new chemotherapy regimens.
Image Credit: Harvard’s Wyss Institute and Harvard SEAS
